How Do Tooth Implants Work: Step-by-Step Guide to Restore Your Smile
Tooth implants work by replacing missing teeth with artificial ones anchored into your jawbone using a titanium post. The process starts with a consultation and involves several stages, including surgical placement, healing, and attaching a natural-looking crown. This guide will explain how do tooth implants work at each step in detail.
Key Takeaways
- Dental implants consist of a titanium screw, abutment, and crown, designed to replicate the look and function of natural teeth.
- Candidates for dental implants must have a fully developed jawbone and good oral health, with lifestyle factors like smoking potentially impacting eligibility.
- Post-procedure care and regular maintenance are crucial for the longevity and success of dental implants, ensuring they remain functional and free from complications.
Understanding Tooth Implants

Dental implants are sophisticated devices designed to replace missing teeth with prosthetics that look, feel, and function like natural teeth. At the heart of a dental implant is a titanium screw, which acts as an artificial tooth root. This metal post is surgically placed into the jawbone, where it integrates with the bone to provide a stable foundation for the new tooth.
The dental implant system consists of three main components: the titanium screw, an abutment, and a crown. The abutment serves as a connector between the implant and the crown, which is the visible part of the new tooth. Crowns are typically made from porcelain or composite materials, chosen for their durability and natural appearance. This structure allows dental implants to closely replicate the function and appearance of real teeth, offering a long-term solution to tooth loss.
Interestingly, the concept of dental implants is not new. Historical records reveal that attempts to replace missing teeth date back thousands of years. However, it wasn’t until the 1950s that modern dental implants, utilizing titanium, were developed, revolutionizing the field of dentistry.
Eligibility for Dental Implants
Not everyone is an ideal candidate for dental implants. The first criterion is a fully developed jawbone, as implants require sufficient bone density to anchor securely. During the initial consultation, your oral health will be assessed to ensure you meet this requirement. Conditions like gum disease, insufficient bone density, or certain medical conditions that affect bone healing could disqualify you from getting implants.
Lifestyle factors also play a crucial role. Smoking, for instance, can significantly reduce the success rate of dental implants due to its adverse effects on oral health and healing. Therefore, it’s imperative to discuss your medical history and lifestyle habits with your dentist to determine your suitability for this procedure.
Initial Consultation and Planning

The journey to a new smile with dental implants starts with a thorough initial consultation, involving a comprehensive evaluation of your oral health and medical history. Your dentist or oral surgeon will review your dental health, check for any untreated gum disease, and assess the need for tooth removal or other preparatory treatments, including dental surgery. Imaging tests like X-rays or CT scans are performed to evaluate the condition of your jawbone and plan the optimal placement areas for the implants.
A detailed treatment plan is then developed, often involving multiple specialists such as oral and maxillofacial surgeons, periodontists, and prosthodontists. Molds of your jaw and teeth ensure the new crowns will fit perfectly and look natural. This meticulous planning phase is critical for the success of the dental implant procedure in oral and maxillofacial surgery.
Bone Grafting and Preparation
A strong, healthy jawbone is key for successful dental implants. However, if your jawbone lacks thickness or is too soft, bone grafting may be necessary to provide a solid foundation. Bone grafting involves transplanting bone tissue to the implant site, which can come from your own body (autograft) or from a donor (xenograft).
The purpose of bone grafting is to ensure that there is enough healthy bone to support the dental implant. This procedure can often be done at the same time as the implant surgery, although in some cases, it may require a separate procedure followed by a healing period of four to six months. This waiting period allows the transplanted bone to integrate with the existing bone, creating a strong base for the implant.
Once the bone graft has sufficiently healed, the site is prepared for implant placement, ensuring the dental implant will be securely anchored and reducing the risk of failure.
Implant Placement Procedure
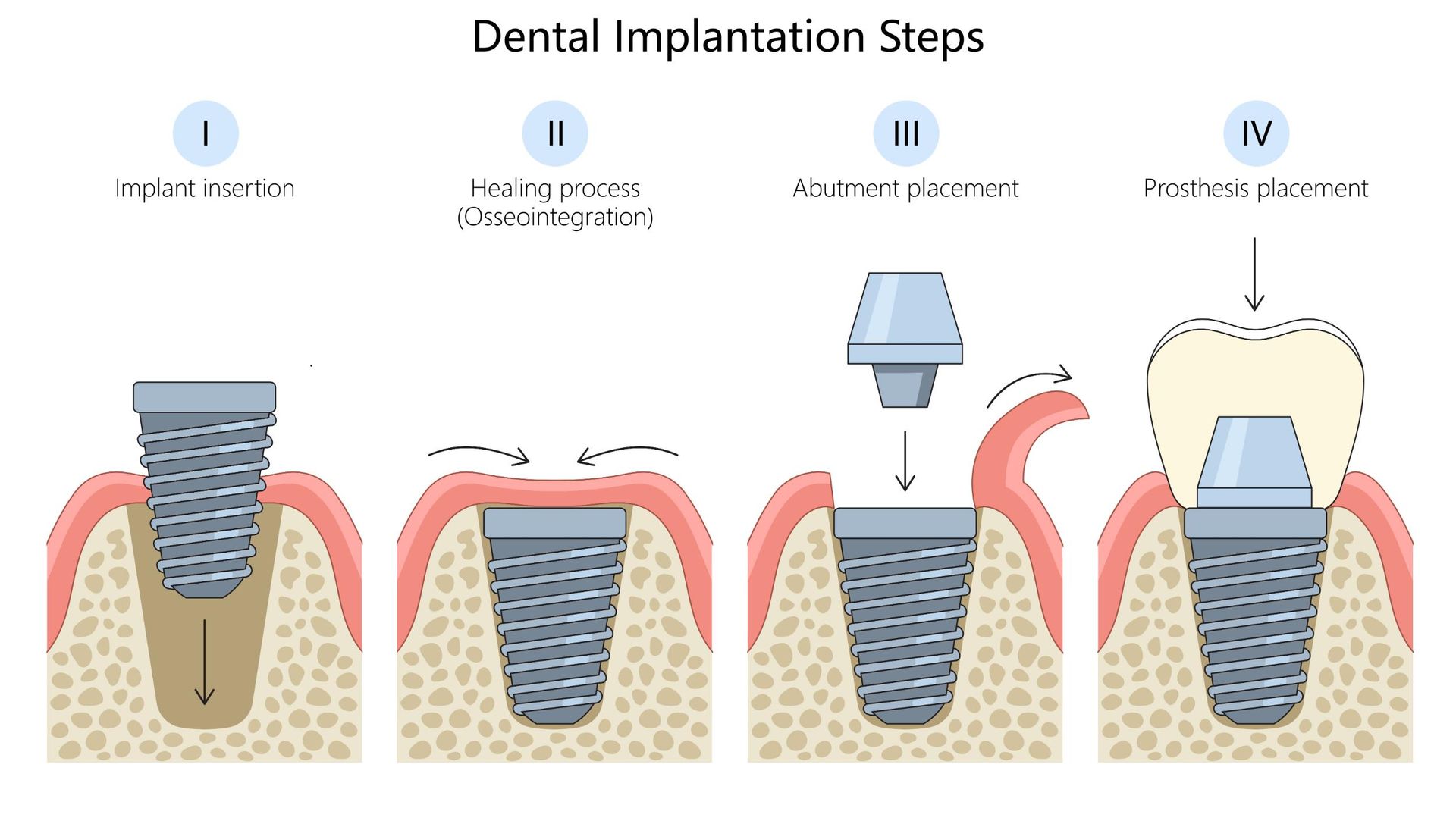
The dental implant placement procedure is a significant step in restoring your smile. Performed under local anesthesia, it involves making an incision in the gums to expose the jawbone, where the oral surgeon then drills precise holes to insert the titanium implant post during dental implant surgery.
After the implant is securely placed, the incision is closed with stitches, and the healing process begins. This period is critical as it allows the jawbone to fuse with the implant, providing a stable foundation for the future crown. The success of this phase largely depends on the body’s ability to heal and integrate the implant.
Osseointegration Process
Osseointegration, a vital part of the dental implant journey, involves the jawbone gradually fusing with the titanium implant, creating a stable and durable anchor for the new tooth. The duration of osseointegration can vary, typically taking between three to nine months, depending on individual healing rates and bone quality.
Successful osseointegration is essential for the long-term stability of the dental implant. It ensures that the implant can withstand the forces of chewing and biting, distributing them evenly across the jawbone and preventing implant failure. This stage is crucial for the durability and functionality of the dental implant.
Abutment Placement
After osseointegration is complete, the next step is placing the abutment, which connects the implant to the crown. This minor procedure, typically performed under local anesthesia, involves reopening the gums to expose the implant. The abutment, typically made from titanium, zirconia, or stainless steel, is then attached to the implant.
After the abutment is placed, the gums need about two weeks to heal. This healing period ensures the gums properly contour around the abutment, creating a natural-looking gum line around the future crown.
Choosing and Placing the Crown
With the abutment in place, the final step involves choosing and placing the crown. Options for artificial teeth include removable, fixed, or a combination, depending on individual preferences and specific dental needs. Temporary crowns may be used while the permanent crown is being fabricated to maintain appearance and function.
The permanent crown is placed once the jawbone is strong enough to support the new natural tooth. This crown is designed to match the natural shape, color, and size of your existing teeth, ensuring a seamless and natural-looking smile.
Post-Procedure Care

Proper post-procedure care is crucial for the success and longevity of dental implants. Immediately after surgery, avoid rinsing or spitting for the first 24 hours and apply ice packs to reduce swelling. A soft-food diet is recommended to aid in healing, and hard or sticky foods should be avoided to prevent damage to the implants.
Good oral hygiene practices, such as daily brushing and flossing, are crucial for preventing infections like peri-implantitis, which can lead to implant failure. Regular dental visits are essential for monitoring the health of the implants and catching any issues early.
Adhering to these care instructions ensures a smooth recovery and long-term implant success.
Benefits of Dental Implants
Dental implants offer numerous benefits, making them a preferred choice for tooth replacement. One of the most significant advantages is their stability and durability compared to traditional dentures or bridges. Unlike dentures, implants do not dislodge and do not require removal for cleaning, providing a more convenient and comfortable solution.
Additionally, with a success rate of over 95%, dental implants work as a reliable option for replacing missing teeth. They also boost confidence in smiling, talking, and eating, ultimately enhancing overall quality of life.
Potential Complications and Risks
While dental implants are generally safe, potential complications and risks must be considered. Infections can occur at the implant site, affecting surrounding teeth and bone. In rare cases, the bone may fail to fuse with the implant, necessitating its removal and retrying the procedure after a few months.
Other risks include minor bleeding, nerve damage, and allergic reactions to implant materials. Monitoring for signs of implant failure and maintaining open communication with your dentist is essential to address any issues promptly.
Maintaining Your Dental Implants
Maintaining dental implants is similar to caring for natural teeth. Brushing with a soft-bristle brush and using low-abrasive toothpaste is recommended. Flossing around the abutments and between teeth is essential to prevent plaque buildup and gum disease. Regular dental check-ups are critical for assessing the health of your implants and ensuring their longevity.
Avoid chewing on hard objects and consider wearing a mouthguard during sports to protect your implants. With proper care, you can get dental implants that last for decades, providing a long-term solution for missing teeth.
Summary
In summary, dental implants are a highly effective and durable solution for replacing missing teeth. From the initial consultation and planning to the final crown placement, each step is crucial for ensuring the success of the implants. Understanding the process and maintaining proper care can lead to a lifetime of confident smiles.
If you’re considering dental implants, consult with a dental professional to determine if you’re a suitable candidate. Embrace the journey to restore your smile and enjoy the numerous benefits that dental implants offer.
Frequently Asked Questions
Orlando Lifestyle Dentistry
How long does the entire dental implant process take?
The entire dental implant process generally takes between six to nine months, influenced by individual healing rates and any necessary additional procedures. Therefore, it is important to plan accordingly for the duration of the treatment.
Are dental implants painful?
Dental implants are not painful during the procedure due to local anesthesia, although some discomfort may occur during the healing process, which can be effectively managed with pain medication.
Can I get dental implants if I have gum disease?
You cannot receive dental implants until your gum disease is treated and managed, as healthy oral tissues are crucial for the success of the implants. Therefore, addressing gum disease should be your first priority.
How do I care for my dental implants?
To care for your dental implants, it is essential to maintain good oral hygiene by brushing with a soft-bristle brush, flossing daily, and attending regular dental check-ups. Additionally, avoid chewing on hard objects and consider wearing a mouthguard during sports to protect your implants.
What are the risks associated with dental implants?
Dental implants carry risks such as infections, nerve damage, minor bleeding, and allergic reactions. Regular monitoring and open communication with your dentist are essential to address any complications promptly.











